What are the signs of severe mold toxicity?
For many people, the term “mold” brings to mind a runny nose or a localized patch of mildew in the shower. However, when exposure becomes chronic and the environment becomes saturated, the situation shifts from a simple irritant to a complex medical challenge.
So, “how do I know if my mold symptoms are severe?” Well, the answer often lies in the transition from localized respiratory issues to systemic mold inflammation. Unlike standard seasonal allergies, severe mold toxicity signs involve the body’s inability to clear out mycotoxin.
In this guide, we will break down the 5 core indicators that your household mold exposure has reached a critical, systemic level:
- Neurological impairment: Beyond brain fog into cognitive decline.
- Chronic respiratory distress: Persistent inflammation that resists standard treatments.
- Systemic inflammatory response: Multi-organ pain and unexplained fatigue.
- Digestive and immune dysfunction: A breakdown of the body’s natural barriers.
- Dermatological and sensory sensitivities: Extreme reactions to light, touch, or skin irritants.
Recognizing these signs early is vital, as prolonged exposure can lead to a heightened state of biotoxicity where the body remains in a cycle of inflammation even after you’ve left the damp environment.
The Big 5 Systemic Symptoms
When mold exposure transitions from an acute irritation to mycotoxin illness, the symptoms become systemic. This means the toxins are no longer just affecting the point of contact (your nose or throat) but are circulating through your bloodstream and affecting multiple organ systems.
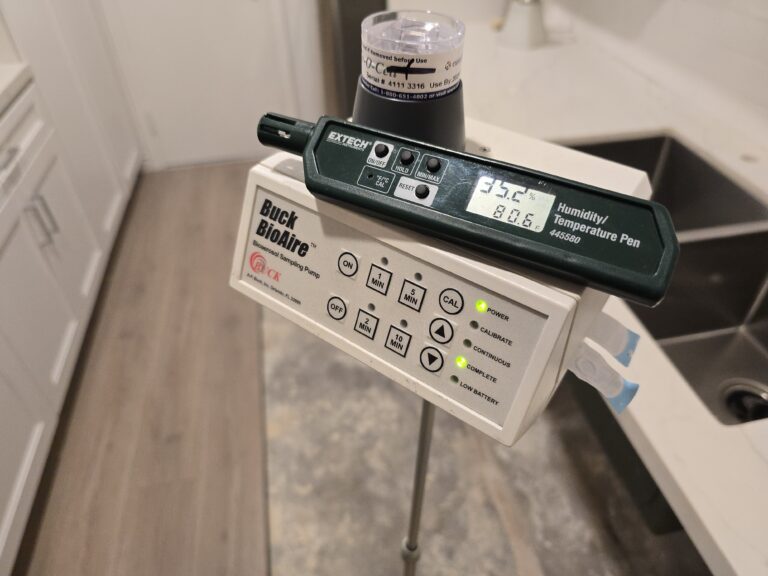
Indoor mold is a significant public health concern, as moisture-damaged buildings can harbor a complex mixture of mold, bacteria, and secondary metabolites that impact indoor air quality.
1. Neurological Brain Fog and Cognitive Decline
One of the most debilitating severe mold toxicity signs is the impact on the central nervous system. Mold-induced brain fog isn’t just feeling tired; it’s a clinical level of cognitive impairment documented in peer-reviewed studies. Patients often report:
- Memory Lapses: Difficulty recalling common words or names.
- “Ice Pick” Headsets: Sharp, stabbing pains in the head that are distinct from standard tension headaches.
- Disorientation: Feeling spaced out or disconnected from your surroundings.
2. Chronic Respiratory Distress
While a mild cough is common, systemic inflammation often leads to dyspnea (shortness of breath) and intense chest tightness. Research indicates that living in damp indoor environments is strongly associated with the exacerbation of asthma and other upper respiratory tract symptoms. If you find yourself gasping for air even without physical exertion, the mold may be triggering a deep inflammatory response in the lung tissue.
3. Dermatological and Ocular Irritation
Mycotoxins can enter the body through the skin or eyes, leading to persistent issues that don’t respond to typical creams or drops.
- Dermatitis: Unexplained skin rashes, hives, or a burning sensation on the skin.
- Photosensitivity: A hallmark of photosensitivity mycotoxins is blurred vision or a sudden inability to tolerate bright lights, often accompanied by red, watering eyes. This occurs because certain mycotoxins can irritate the optic nerve and disrupt the brain’s ability to process visual contrast.
4. Musculoskeletal Pain
A defining feature of systemic mold inflammation is mold joint pain. Unlike an injury that stays in one place, mold-related pain is often migratory. Some individuals also experience fine muscle tremors or “fasiculations” (involuntary twitches) as the toxins interfere with nerve signaling to the muscles.
5. Extreme Fatigue and Mitochondrial Stress
This is more than just being “worn out.” It is a profound, cellular lethargy. Emerging studies suggest that mycotoxins can cause mitochondrial stress, effectively “unplugging” your body’s energy production. This results in chronic exhaustion that does not improve with sleep or caffeine, often leaving patients bedridden for days at a time.
Mold Allergy vs. Mold Toxicity: The Critical Distinction
A common mistake many homeowners make is treating mold as a simple allergen. Understanding the difference between an allergy and toxicity is vital for getting the correct medical treatment, as the diagnostic paths and biological mechanisms are entirely different.
While many molds are common allergens, “toxic mold” refers to specific species that produce mycotoxins, which can cause illness through pathways other than a standard allergic response.
The Biological Breakdown
| Feature | Mold Allergy | Mold Toxicity (Mycotoxin Illness) |
| Mechanism | An overreaction of the immune system to inhaled spores. | A chemical poisoning from toxic secondary metabolites (mycotoxins). |
| Primary Testing | IgE mold testing (Skin prick or blood tests for immediate hypersensitivity). | IgG mold testing (Looking for long-term exposure) and Urinary Mycotoxin panels. |
| Primary Organs | Eyes, nose, throat, and lungs. | Brain, nervous system, liver, and gut. |
| Response | Usually subsides shortly after leaving the area or taking antihistamines. | Can persist for weeks or months after removal due to “toxic load” in fatty tissues. |
Why the Distinction Matters
If you are suffering from systemic mold inflammation, a standard allergy test may come back negative. This is because your body isn’t necessarily allergic to the mold; rather, it is being biochemically overwhelmed by the toxins the mold is off-gassing.
The 25% Genetic Blind Spot
A groundbreaking discovery in the field of environmental medicine reveals why two people can live in the same moldy house, yet only one gets deathly ill. Approximately 25% of the population carries specific HLA-DR genetic mold susceptibility markers.
In a healthy immune system, the body identifies mycotoxins, tags them as invaders, and flushes them out via the liver and digestive tract. However, in those with the susceptible HLA-DR gene:
- The body fails to recognize mycotoxins as foreign.
- Instead of being eliminated, the toxins circulate indefinitely.
- This triggers a “cytokine storm,” leading to the systemic mold inflammation we see in chronic cases.
The Biotoxin Pathway Effect
When you have CIRS mold illness, the toxins begin to damage the body at a cellular level. This often results in a drop in Melanocyte-Stimulating Hormone (MSH), a master regulator in the brain. When MSH levels fall, it creates a “domino effect” of symptoms:
- Sleep fragmentation: Chronic insomnia regardless of how tired you are.
- Leaky gut: Increased intestinal permeability and new food sensitivities.
- Hormonal imbalance: Dysregulation of ADH (Antidiuretic Hormone), leading to frequent urination and excessive thirst.
- Chronic pain: Suppressed endorphin production, making the body hypersensitive to pain.
What to Tell Your Doctor
When you’re looking for how to talk to your doctor about mold, your goal is to bridge the gap between your environment and your internal symptoms using objective evidence.
The Exposure Timeline
Create a simple log that correlates your health with your location. This helps you provide your doctors with accurate information:
- Onset: When did symptoms start? Does it align with moving into a new home or a specific water event (like a burst pipe)?
- Relief: Do symptoms improve when you are away from the home for more than 48 hours (e.g., on vacation or at work)?
FAQ: Your Questions Answered
To help you navigate the complexities of mycotoxin illness, we’ve gathered the most frequent questions from our community. Capturing these answers early can be the key to a faster recovery.
1. Can mold exposure cause permanent damage?
In many cases, the body is remarkably resilient. However, if systemic mold inflammation is left untreated for years, it can lead to chronic conditions like secondary autoimmune disorders or permanent respiratory scarring.
2. How long does it take for mold to affect your lungs?
It varies. For those with a mold allergy, symptoms like wheezing can start within minutes. For mycotoxin illness, the timeline is usually longer, often requiring weeks or months of chronic exposure for the toxins to build up to a symptomatic level in the tissues.
3. Will symptoms go away once the mold is removed?
For approximately a majority of the people, removal from the environment leads to a steady recovery. However, some people may require a clinical detoxification protocol to assist the body in clearing the stored biotoxins.
Conclusion: Taking Control of Your Environment
Identifying severe mold toxicity signs is the first step toward reclaiming your health. Whether you are dealing with mold-induced brain fog or migratory mold joint pain, remember that your symptoms are a biological signal that your environment is no longer serving you.
Severe household mold exposure is a silent thief of vitality, but with the right diagnostic tools and a clear remediation plan, recovery is possible. Don’t wait for the symptoms to become debilitating; act as soon as you suspect your home’s health is impacting your own.
Continue Your Research
To further understand the relationship between your home and your health, explore these related guides: